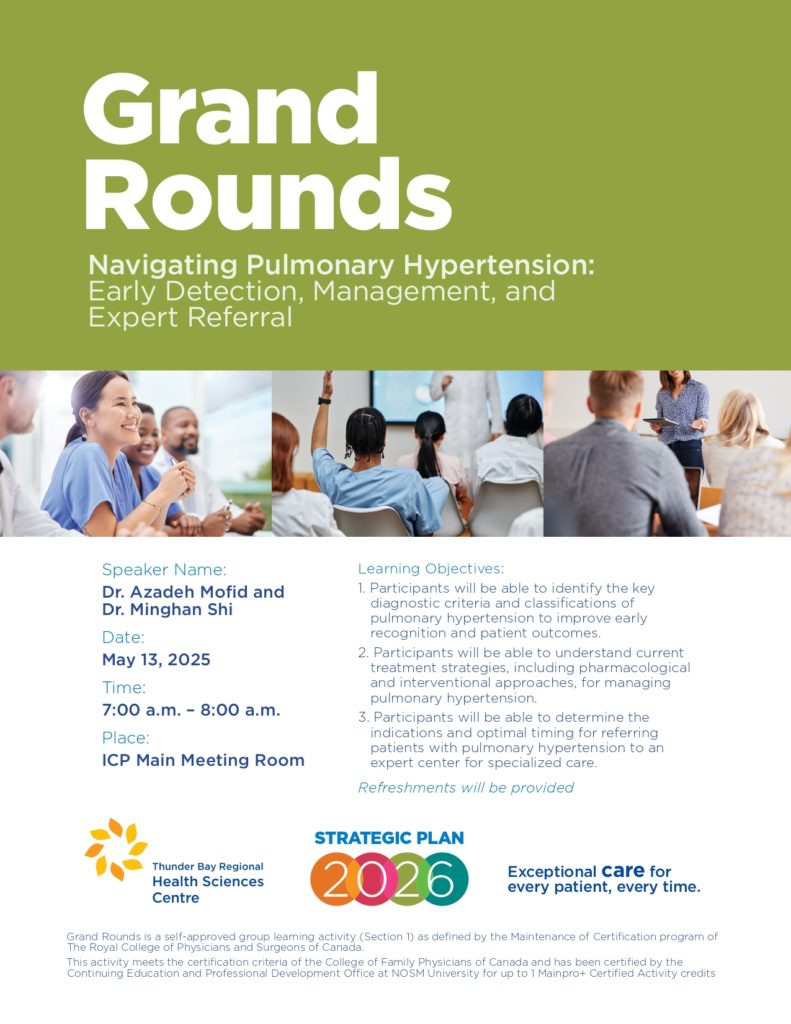
Grand Rounds (May 13)



Shared on behalf of Medical and Academic Affairs
I am pleased to announce that Cassidy Tackacs has accepted a contract position as Physician Retention and Relations Specialist covering for Samantha Olsen during her leave.
Cassidy most recently worked as a Human Resources Officer – Recruiter at Dilico Anishinabek Family Care and is a graduate of Lakehead University with an Honours Bachelor of Commerce (Marketing and Human Resources Management). She brings with her experience in full cycle recruitment and retention activities and exceptional administrative skills. We are thrilled to welcome her to our Medical and Academic Affairs portfolio where she will work alongside Laurel Knowles, Physican Recruitment Specialist and Dr. William Harris as he transitions to the role of Associate Vice President, Physician Recruitment and Retention.
Cassidy begins on Monday, May 12, 2025. Some of her early priorities will be updating and strengthening our physician orientation processes and follow up, and continuing to expand retention activities in a strategic way. She will continue to support physician payment processes as well and we hope to lean into her marketing background to continue improving our communication opportunities.
Please join us in welcoming Cassidy to our team!
This week is Emergency Preparedness Week! This year’s theme is “Be Prepared. Know your Risks”. The intent of the theme is to encourage us all to understand the risks in our area and learn what actions we can take to protect ourselves, our families, and our community.
Here at TBRHSC we recognize the importance of running regular emergency preparedness drills and exercises to help us test and validate our response plans, policies, procedures, and capabilities. They also help us identify strengths, areas for improvement, and potential best practices.
Every year Interprofessional Education and Emergency Preparedness run dozens of drills and exercises; most recent being last week’s Code White drill.
Thank you to everyone who takes the time to engage in these learning opportunities throughout the year! Whether as direct participants or as planners, observers, and evaluators, your contributions matter.
Check out the tentative list of drills and exercises we hope to achieve with your support later this year:
Note: the above list doesn’t include tabletop exercises or upcoming collaborations between TBRHSC and external stakeholders (e.g., City of Thunder Bay’s annual emergency management exercise).
Future goals include improving our ability to capture who has attended mock codes and exercises, as well as improving our methods of capturing participant feedback. We are also dedicated to enhancing and formalizing our debriefing processes.
How to request a drill?
For general inquiries, reach out to Mēsha Richard, Lead, Emergency Preparedness (Mesha.Richard@tbh.net) or contact Brittney McLaughlin (Brittney.McLaughlin@tbh.net Mock Code Blue), Holly Freill (Holly.Freill@tbh.net Mock Code White), or Jennifer Gadioma (Jennifer.Gadioma@tbh.net Mock Code Pink & NRP).
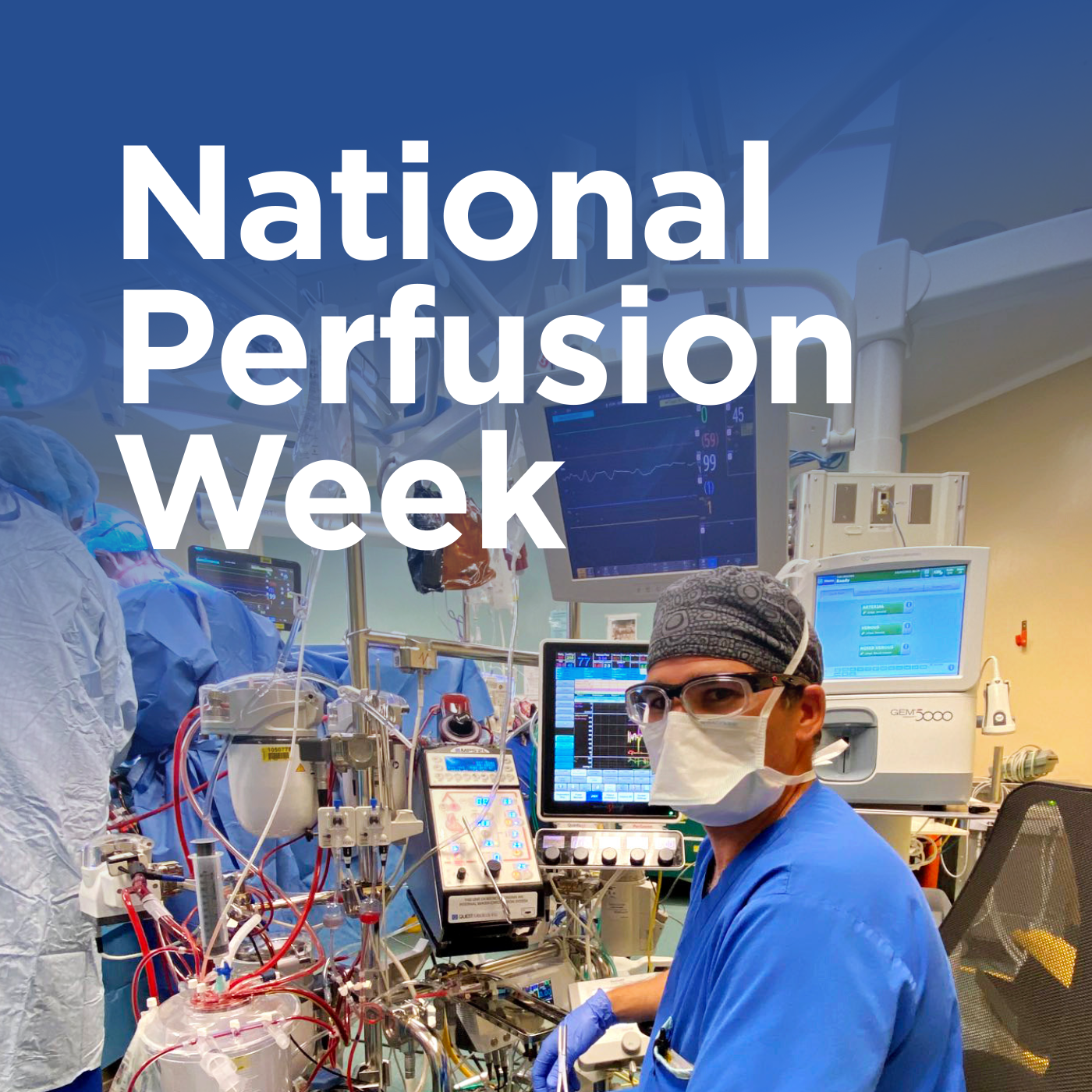
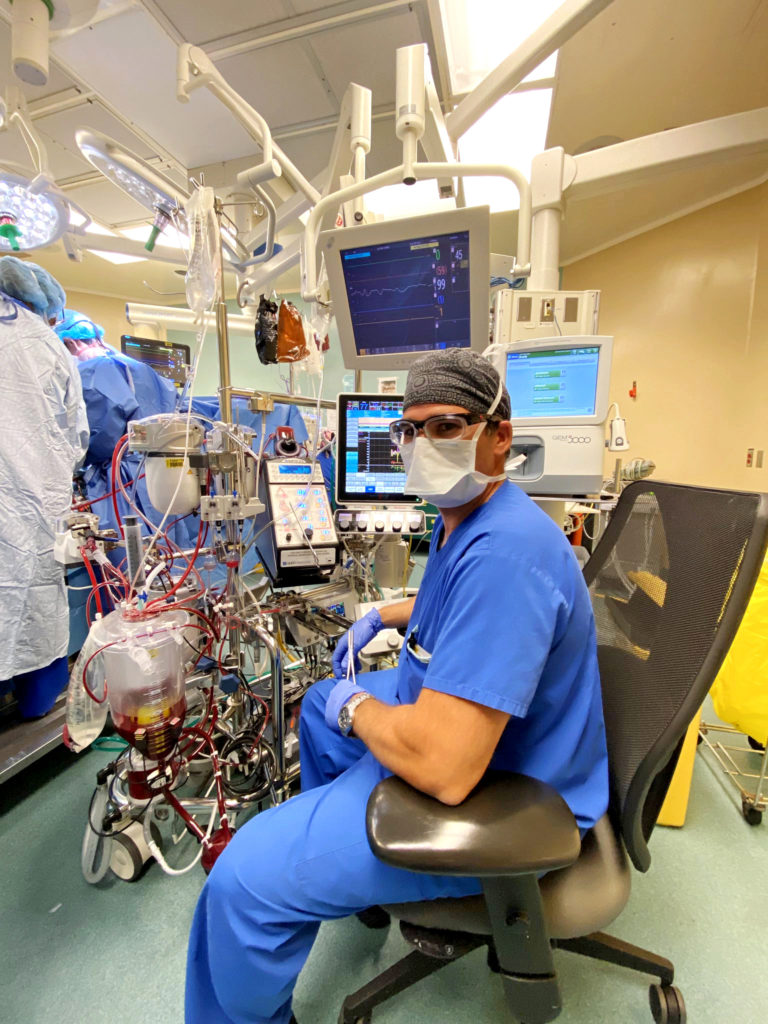
Cardiovascular perfusionists play a vital and intricate role as integral members of the interprofessional operating room team, working seamlessly alongside cardiac surgeons and anesthesiologists to ensure optimal patient outcomes during complex surgical procedures. Their responsibilities include the management and operation of sophisticated technologies such as the heart-lung machine, which is crucial for conducting cardiopulmonary bypass—a process that temporarily takes over the function of the heart and lungs during surgery.
In celebration of National Perfusion Week, we take great pride in honouring the exceptional skill and dedication of cardiovascular perfusionists, whose expertise plays a crucial role in patient care. This week, we spotlight four remarkable staff members who will join our team at the Thunder Bay Regional Health Sciences Centre (TBRHSC). These talented professionals are poised to make significant contributions as they prepare for the highly anticipated launch of the Cardiovascular Surgery Program in early 2028. Their commitment to advancing healthcare and improving patient outcomes exemplifies the spirit of excellence we aspire to in our facilities.
Scott Longridge completed the Cardiovascular Perfusion Program at the Michener Institute of Education at the University Health Network (UHN) in March 2018. He has dedicated many years to Thunder Bay Regional Health Sciences Centre (TBRHSC) and currently applies his expertise at the Peter Munk Cardiac Centre (PMCC) at UHN, one of Canada’s leading cardiac care institutions, allowing Scott to further refine his expertise in a collaborative environment that prioritizes patient outcomes and innovative practices in cardiac health.

We would like to take a moment to recognize Amanda Sanche, who embarked on the two-year cardiovascular perfusion studies at the Michener Institute of Education at the UHN in September 2023. Throughout her rigorous academic journey, Amanda has demonstrated exceptional dedication and resilience, culminating in her recent completion of a Master of Science degree in Cardiovascular Perfusion. Starting this month, Amanda will transition into her first professional role as a Cardiovascular Perfusionist at the PMCC, where she will play a crucial role in supporting patients undergoing complex cardiac surgeries. With this significant achievement, we extend our heartfelt congratulations to Amanda for her hard work and commitment to advancing her career in cardiovascular medicine. We wish her all the best as she embarks on this exciting new chapter!

In September 2024, Grace Lovis embarked on her first year in the highly regarded Cardiovascular Perfusion Program at the Michener Institute of Education at UHN. With a strong commitment to academic excellence and a deep passion for patient care, Grace is poised to develop the critical skills necessary for this demanding field. Her dedication, paired with her determination to contribute positively to the healthcare team, positions her to become an invaluable asset to our organization upon the successful completion of her training.

With years of critical care experience, Eve Dillion has recently been accepted as the final staff member to join the Cardiovascular Perfusion Program at the Michener Institute of Education at UHN for the 2025/2026 academic year. Alongside her peers, she will embark on the journey to earn her Master of Science degree in Cardiovascular Perfusion, equipping her with the expertise to support patients undergoing cardiovascular surgery. Congratulations to Eve on this outstanding achievement!
The collective dedication to learning, expertise, and commitment to delivering safe and comprehensive perfusion therapy that these individuals embody will be invaluable to the TBRHSC and the diverse patient population we serve. As they prepare to contribute to our cardiovascular program, we extend our best wishes and look forward to welcoming them to our team.
Join us this week in acknowledging and appreciating the essential work that perfusionists undertake in the operating room, where their skills and knowledge significantly impact patient survival and recovery.
Learn more about cardiovascular perfusion at these online resources:
This week is Emergency Preparedness Week! This year’s theme is “Be Prepared. Know your Risks”. The intent of the theme is to encourage us all to understand the risks in our area and learn what actions we can take to protect ourselves, our families, and our community.
Emergency Preparedness at TBRHSC
At TBRHSC, our Emergency Preparedness Committee (EPC) works to ensure that we have the capacity to effectively prepare for, respond to, and recover from emergencies. The EPC is comprised of over 20 representatives from various programs and services and is responsible for providing oversight and leadership related to hospital emergency preparedness.
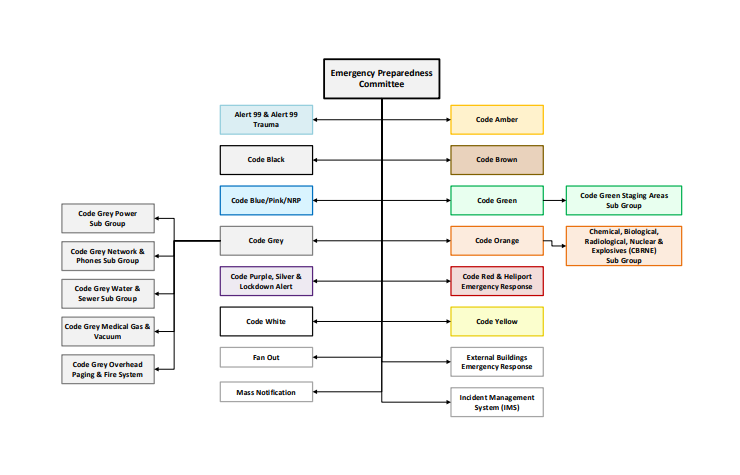
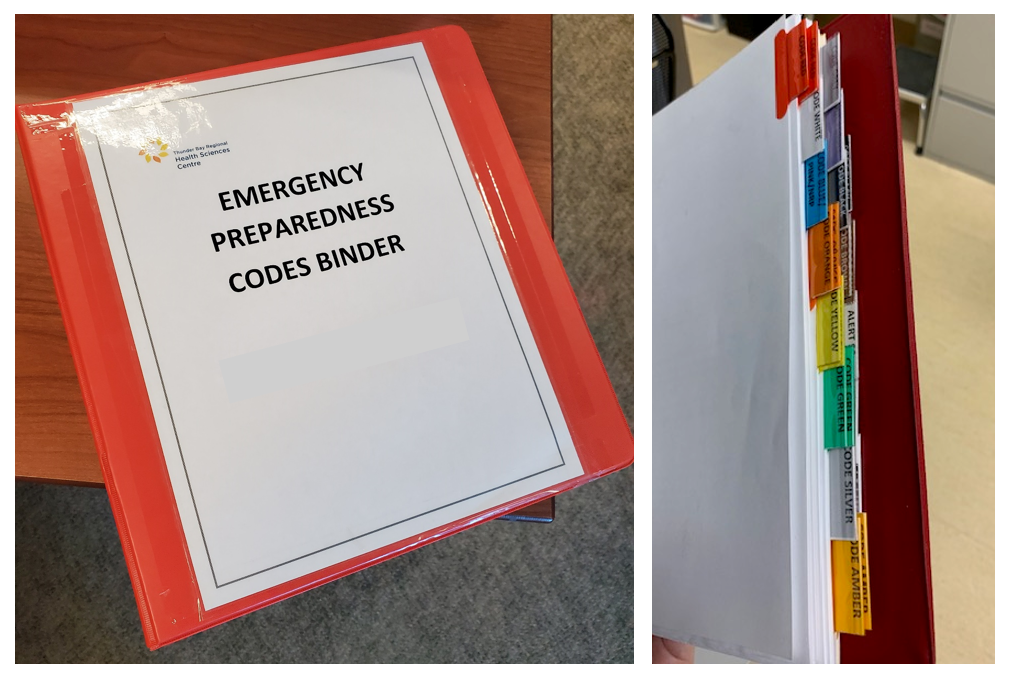
TBRHSC follows the Ontario Hospital Association (OHA) standardized Emergency Colour Code system. Each colour code (as well as Alert 99 and Lockdown) has an Executive Sponsor (who is also a member of the EPC) and working group assigned to maintain the associated policy, review key incidents, and identify training and exercise opportunities. The Manager, Emergency Preparedness, Switchboard & Security and the Lead, Emergency Preparedness work closely with all these groups (see below for working group reporting structure).
See the EPC’s Terms of Reference document via the link for a better understanding.
If you have questions, please reach out to your manager or Mēsha Richard, Lead, Emergency Preparedness (ext. 6552 or mesha.richard@tbh.net)

Please be advised that the Regional Cancer Care Northwest will be closed for the entire day on Friday, May 9, 2025, to allow staff to participate in the Community Oncology Professional Education Workshop.
For inquiries, please contact Lori Hygaard at lori.hygaard@tbh.net.


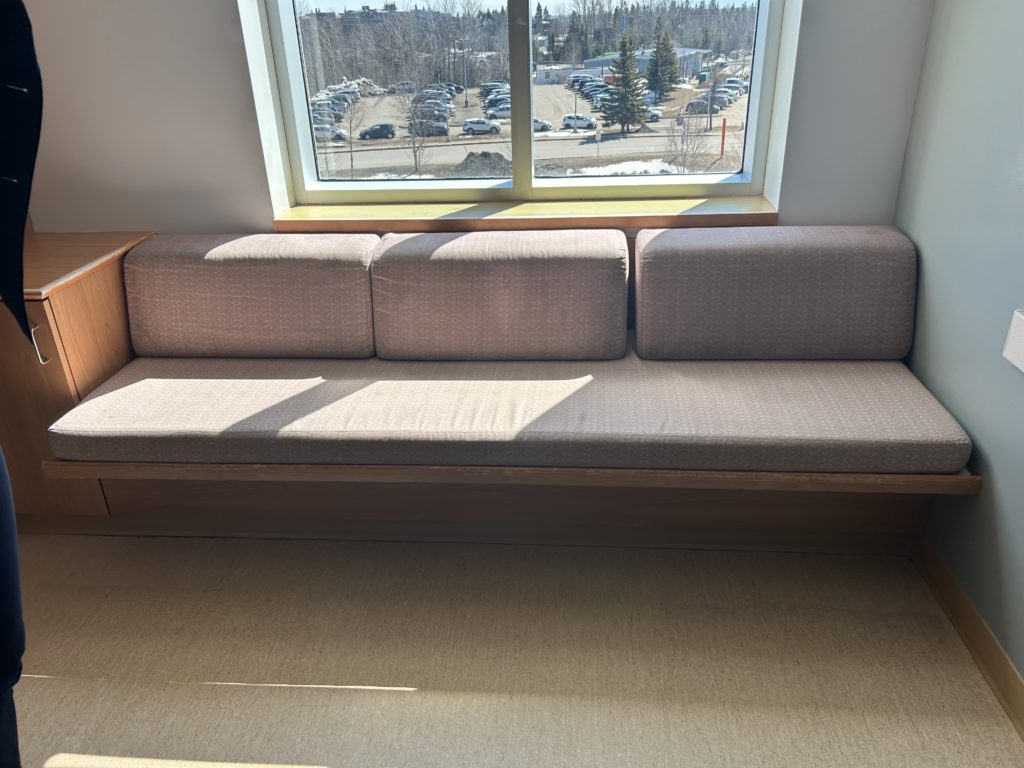
We want to hear from you! We are seeking your input on the purchase of new bedside visitor bench cushions for our inpatient private rooms.
We want to ensure that the new cushions meet the needs and preferences of both staff and visitors. To gather your feedback, we invite you to a viewing session on Tuesday, May 6 from 11:00 a.m. to 12:00 p.m. in the ICP-Video Conference Room (2171).
During this time, you will have the opportunity to see several options and cast your vote for your preferred choice. Please share this information with all staff members. Everyone is encouraged to stop by and check out the options.
This week is Emergency Preparedness Week! This year’s theme is “Be Prepared. Know your Risks”. The intent of the theme is to encourage us all to understand the risks in our area and learn what actions we can take to protect ourselves, our families, and our community.
Emergency Preparedness at TBRHSC
Did you know that at TBRHSC, Emergency Preparedness has its own dedicated iNtranet page? It’s true! Be #ReadyforAnything by reviewing our safety huddles, posters, and training videos. Check it out on the iNtranet under Departments > Emergency Preparedness and Security > Emergency Preparedness or via this link, and follow along as we gradually build up this resource with new material!
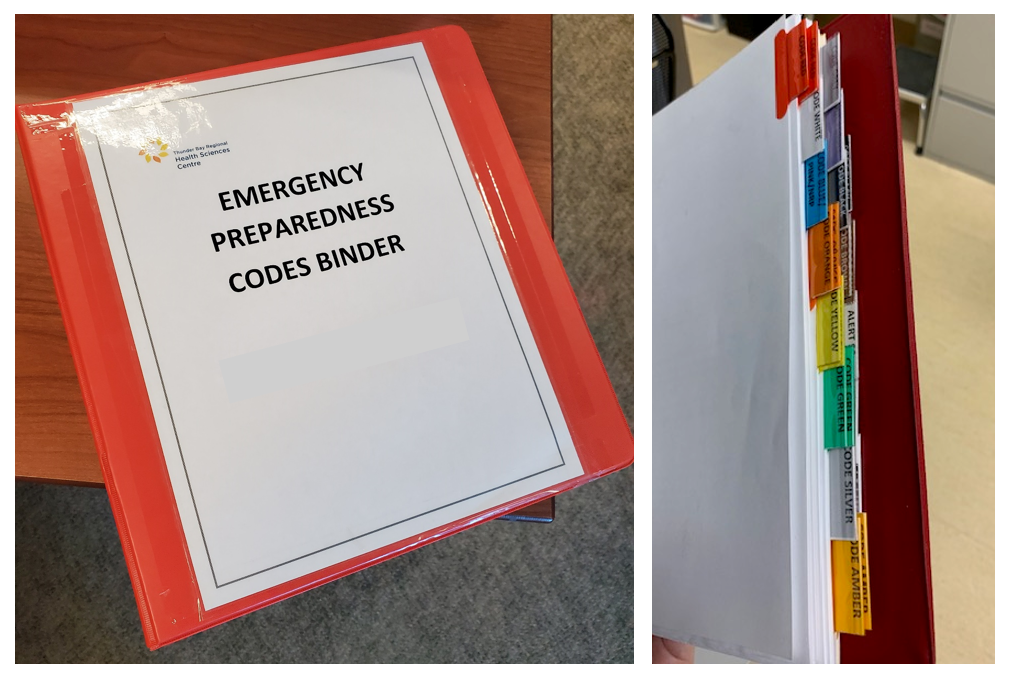
And don’t forget to periodically review our emergency colour code policies and your departmental sub-plans. Emergency code policies are located:
Our emergency colour codes and alerts aren’t meant to be a secret. Want to share with patients and visitors? No problem! Turn to page 25 of the Patient Care Resource booklet or direct them to https://tbrhsc.net/home/information-services/emergency-codes/.
If you have questions, please reach out to your manager or Mēsha Richard, Lead, Emergency Preparedness (ext. 6552 or mesha.richard@tbh.net).
It is National Safety and Health Week (May 5-10). Join us in recognizing National Safety and Health Week, an important initiative dedicated to raising awareness about workplace safety! This week-long event emphasizes the crucial role that safety plays in our everyday work environments. From preventing injuries to fostering overall well-being, it’s essential that we all commit to prioritizing safety measures every day. Whether you’re working on the frontline or in an administrative role, there are steps you can take to protect yourself and your colleagues.
Check out the iNtranet for more information on the Occupational Health and Safety department’s quiz and scavenger hunt. Three prizes will be awarded for quiz submissions. The winning team of the scavenger hunt will receive a “lunch party” for their department! Plus, prizes will be awarded throughout the week in relation to secret safety walkabouts.
To learn more about National Safety and Health Week, click here.